The Centers for Medicare & Medicaid Services (CMS) is supporting clinicians on the front lines by getting red tape out of the way so the healthcare delivery system can focus on the 2019 Novel Coronavirus (COVID-19) response. CMS is implementing additional extreme and uncontrollable circumstances policy exceptions and extensions for upcoming quality measure reporting and data submission deadlines for the following CMS programs:
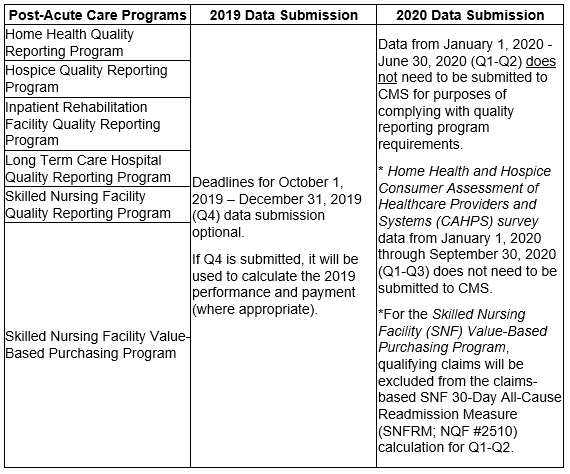
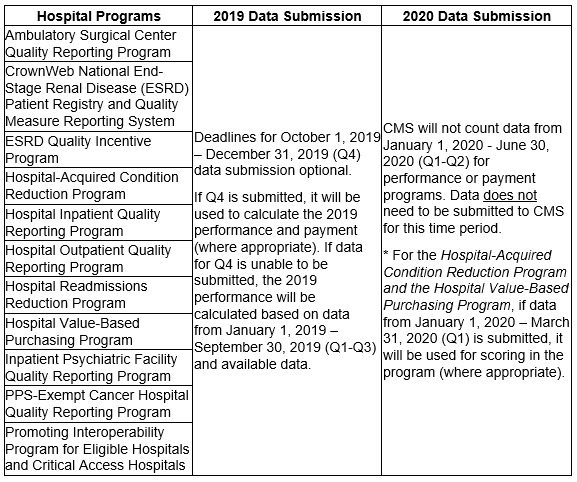
CMS is granting exceptions and extensions to assist healthcare providers and suppliers while they direct their resources toward caring for their patients and ensuring the health and safety of patients and staff. For those programs with data submission deadlines in April and May 2020, submission of those data will be optional based on the facility’s choice to report. In addition, no data reflecting services provided January 1, 2020-June 30, 2020 will be used in CMS’s calculations for the Medicare quality reporting and value-based purchasing programs in order to reduce providers’ data collection and reporting burden as they are responding to the COVID-19 pandemic.
CMS recognizes that quality measure reporting may not be reflective of performance for measures such as cost, readmissions and patient experience during this time of emergency and seeks to hold organizations harmless for data during this period. CMS will continue to monitor the situation and adjust reporting periods and submission deadlines accordingly. More detailed information about changes to each of these quality reporting programs will be provided soon.
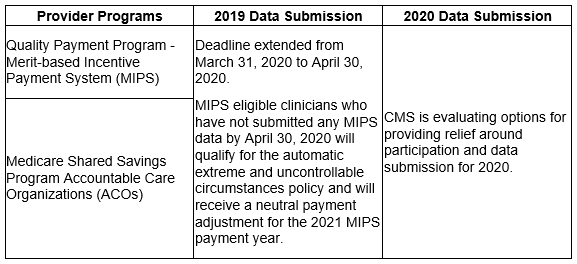
Quality Payment Program
2019 MIPS Submission Deadline Extended: Submit 2019 Data by April 30, 2020
The 2019 MIPS data submission deadline will be extended by 30 days to April 30, 2020. If you have already submitted MIPS data or if you submit MIPS data by April 30, 2020, you will be scored and receive a MIPS payment adjustment based on the data you submit. Many MIPS eligible clinicians have performed very well in the MIPS program in previous years. If you need to revise any data that has already been submitted you can still make changes by logging into qpp.cms.gov by the new deadline.
2019 MIPS Automatic Extreme and Uncontrollable Circumstances Policy Update
MIPS eligible clinicians who have not submitted any MIPS data by April 30, 2020 do not need to take any additional action to qualify for the automatic extreme and uncontrollable circumstances policy. These clinicians will be automatically identified and receive a neutral payment adjustment for the 2021 MIPS payment year. All four MIPS performance categories for these clinicians will be weighted at zero percent, resulting in a score equal to the performance threshold, and a neutral MIPS payment adjustment for the 2021 MIPS payment year. However, if a MIPS eligible clinician submits data on two or more MIPS performance categories, they will be scored and receive a 2021 MIPS payment adjustment based on their 2019 MIPS final score.
CMS will continue monitoring the developing COVID-19 situation and assess options to bring additional relief to clinicians and their staff so they can focus on caring for patients.
For More Information
Please reference the 2019 QPP Data Submission User Guide. CMS also has up to date information about its programs and response to COVID-19 on the Current Emergencies page.
For Quality Payment Program questions you can contact 1-866-288-8292, Monday through Friday, 8:00 AM-8:00 PM ET or by e-mail at: [email protected].
*Customers who are hearing impaired can dial 711 to be connected to a TRS Communications Assistant.




